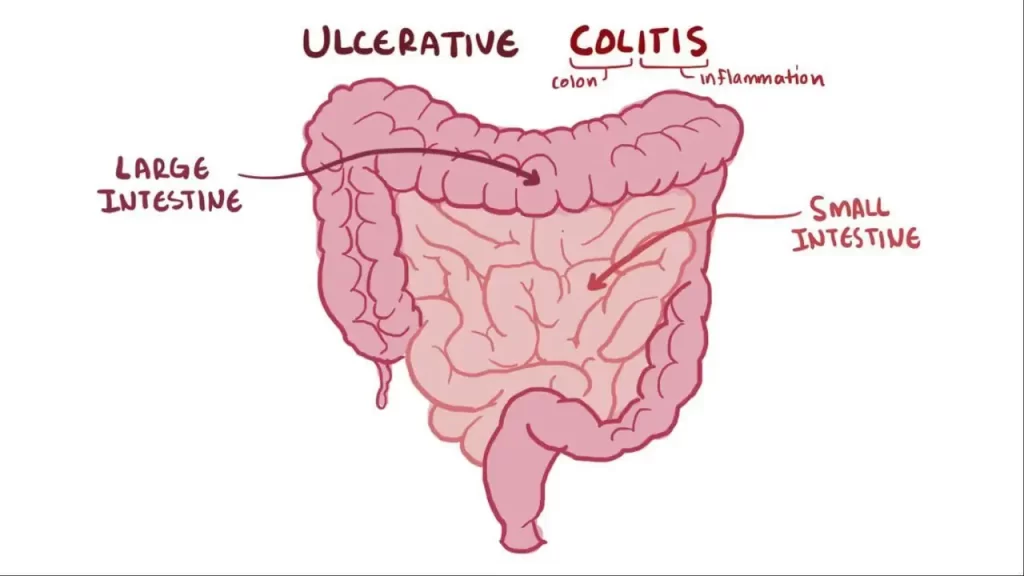
The large intestine, or colon, is the final part of your digestive system (see the image below). By the time food has passed through the 6.5 metres of your small intestine and reaches your colon, most of it has been absorbed and only waste products are left. It is the job of your colon to absorb the excess water, as well as some fibre and potassium, from the waste and move the waste to the rectum. This becomes your stools (poos).
Inflammatory bowel disease (IBD) is a medical term use to describe a group of conditions. Which the intestine becomes inflamed (red and swollen). There are two major types of IBD and they require different treatments.
- Crohn’s disease can occur in any part of your intestine.
- Ulcerative colitis only affects your large intestine (colon). Small ulcers can develop on the colon’s lining, and can bleed, produce pus and become inflamed.
Note that IBD should not be confused with irritable bowel syndrome (IBS). Which is a different condition requiring different treatment.
The exact cause of ulcerative colitis is unknown. The following possible causes have been suggested:
- Immune system
- Ulcerative colitis is thought to be a type of autoimmune disease, in which the body’s immune system (infection fighting system) malfunctions and attacks the tissues of the bowel. This results in swelling and redness (inflammation) of body tissue in the infected area. It’s also been suggested that no infection is involved and the immune system may just malfunction by itself, or that there’s an imbalance of bacteria within the bowel.
- Genes
- It also seems inherited genes are a factor in the development of ulcerative colitis. If your first degree relative (parent, brother, sister, child) has colitis, this can double your lifetime risk. Levels of ulcerative colitis are also a lot higher in people of European or African descent, which also suggests that genetics are a factor.
The most common symptoms are bloody diarrhoea (blood on runny poo), frequent passing of stools and/or an urgent need to pass stools (poos). Occasionally some people may have pain in the lower abdomen (tummy/puku area).
More severe symptoms include weight loss, anaemia, loss of appetite, tiredness, feeling low in mood and slower than usual growth (which is more noticeable in younger people).
The severity of symptoms varies between people and depends on. How much of the rectum and colon is inflamed and how bad the inflammation is. Some people experience their first ulcerative colitis-like symptoms when they are attempting to stop smoking but this goes away with time.
If you have any symptoms of ulcerative colitis and not diagnosed or your medication is not working well for you, see your GP.
Flare-up
Some people may go for weeks or months with very mild symptoms, or none at all (remission), followed by periods where the symptoms are particularly troublesome (flare-ups or relapses). In some cases, a flare-up can be linked to specific cause such as a change of medication. Certain food, however in many cases a specific cause is not found.
During a flare-up, some people with แทงบอล UFABET ราคาดีที่สุด ไม่มีขั้นต่ำ ulcerative colitis also experience symptoms elsewhere in their body. For example, some people develop:
- painful and swollen joints (arthritis)
- mouth ulcers
- areas of painful, red and swollen skin
- irritated and red eyes.